The young population, encompassing adolescents and young adults, faces a myriad of challenges as they navigate the complexities of life. Among these challenges, the correlation between trauma and addiction stands out as a critical area of concern. Scientific literature consistently highlights the profound impact of trauma on the development of addictive behaviours in this demographic. In this blog, we delve into the intricate relationship between trauma and addiction in the young population and emphasize the pivotal role of a trauma-informed approach in conceptualizing and treating addiction. We will also explore how VEDA Rehabilitation and Wellness embraces a holistic methodology to address the unique needs of the young population in their journey toward recovery.
The Correlation between Trauma and Addiction:
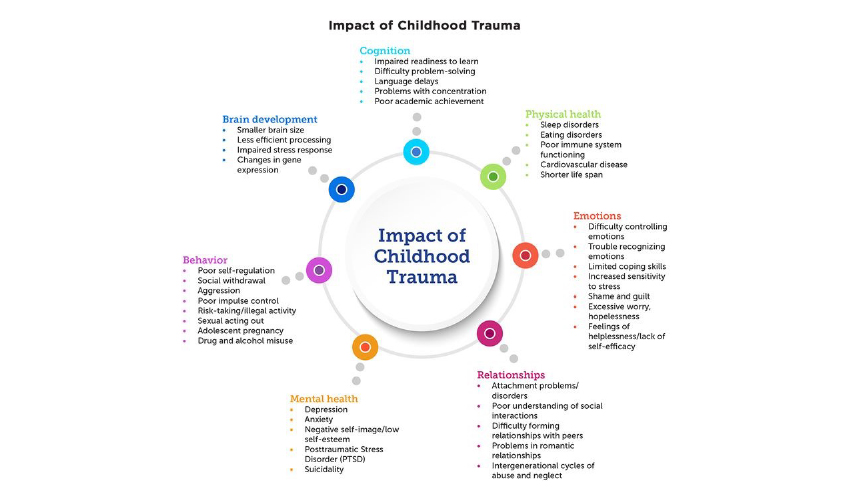
Childhood is a formative period where experiences shape the foundation for a person’s future. However, when these experiences include trauma, the impact reverberates across various facets of a child’s development. This blog explores the profound effects of traumatic experiences during childhood on cognitive, emotional, psychological, spiritual, and physical development, shedding light on the complex interplay between early adversity and holistic well-being.
Cognitive Development:
1. Impaired Executive Functioning:
Childhood trauma can hinder the development of executive functions such as attention control, working memory, and cognitive flexibility. This impairment may manifest as difficulties in problem-solving, decision-making, and overall cognitive adaptability.
2. Learning and Academic Challenges:
The cognitive impact of childhood trauma often extends to academic performance. Children who have experienced trauma may struggle with concentration in school, leading to challenges in learning and academic achievement.
Emotional Development:
1. Difficulty Regulating Emotions:
Traumatic experiences can disrupt the development of emotional regulation skills. Children exposed to trauma may find it challenging to manage and express their emotions appropriately, leading to outbursts, mood swings, or emotional withdrawal.
2. Increased Risk of Mental Health Disorders:
The emotional toll of childhood trauma is a significant factor in the development of mental health disorders, including anxiety, depression, and post-traumatic stress disorder (PTSD). These conditions can persist into adulthood if not addressed early.
Psychological Development:
1. Impact on Self-Esteem and Identity:
Childhood trauma may contribute to a distorted sense of self and low self-esteem. Individuals who have experienced trauma may grapple with feelings of shame, guilt, or worthlessness, affecting their overall psychological well-being.
2. Difficulty Forming Healthy Relationships:
Trauma can influence the ability to form and maintain healthy relationships. Individuals with a history of childhood trauma may struggle with trust issues, intimacy, and communication skills, impacting their interpersonal connections.
Spiritual Development:
1. Loss of Trust and Meaning:
Childhood trauma can erode a child’s sense of trust, both in others and in larger existential beliefs. This loss of trust can extend to a diminished sense of meaning and purpose in life, affecting the spiritual dimension of development.
2. Journey Toward Healing:
While trauma may disrupt spiritual development, the process of healing can lead to a rediscovery of meaning and a deeper connection with one’s sense of self and others.
Physical Development:
1. Impact on Brain Structure and Function:
Childhood trauma can alter the structure and function of the brain, particularly in areas related to stress response and emotional regulation. This can have long-term consequences for physical health, including an increased risk of chronic conditions.
2. Health-Compromising Behaviors:
Coping mechanisms developed in response to trauma, such as substance abuse or self-harm, can have detrimental effects on physical health. These behaviours may serve as maladaptive attempts to cope with the emotional and psychological consequences of trauma and addiction is one such maladaptive coping.
Trauma and Dysregulated Stress System:
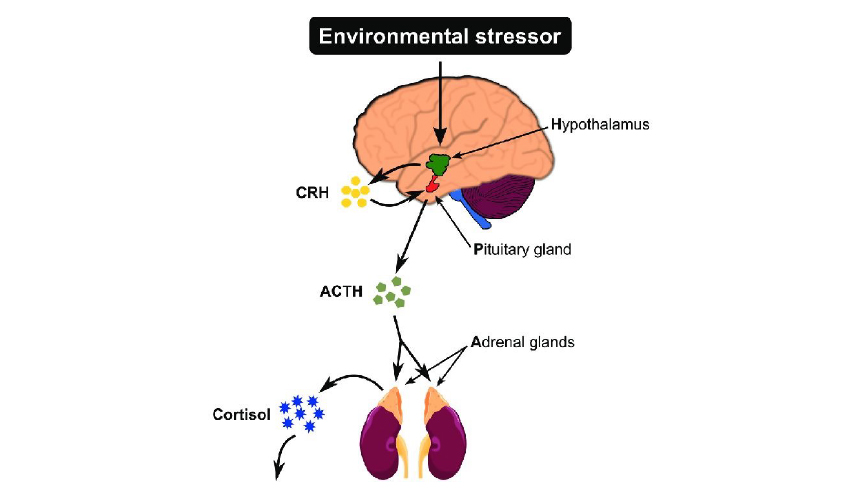
The HPA axis is a crucial part of the body’s stress response system. When an individual encounters stress or a threatening situation, the hypothalamus, a region in the brain, releases a hormone called corticotropin-releasing hormone (CRH). This hormone signals the pituitary gland to produce adrenocorticotropic hormone (ACTH), which, in turn, prompts the adrenal glands to release cortisol, the primary stress hormone.
1. Young individuals experiencing trauma:
Traumatic experiences activate the stress response system in the body, particularly in the HPA axis.
2. Stress systems in a constant state of imbalance:
Trauma can lead to a dysregulated stress response within the HPA axis. Instead of the typical ebb and flow of the stress response, individuals who have experienced trauma may find their HPA axis in a constant state of activation, with elevated levels of cortisol persisting over time.
3. Making them more susceptible to seeking solace in addictive substances or behaviours as a coping mechanism:
The constant activation of the HPA axis and the prolonged exposure to elevated cortisol levels can contribute to heightened vulnerability. In an attempt to cope with the overwhelming stress or emotional pain caused by trauma, individuals may be more inclined to turn to addictive substances or behaviours. This is because substances like drugs or certain behaviours can temporarily alleviate the distressing feelings associated with trauma, providing a perceived sense of solace or escape.
Depersonalization and Numbness:
Depersonalization, a common response to trauma, involves feeling detached or disconnected from oneself, almost as if observing one’s own life from the outside. This dissociative experience can have significant implications, including the development of emotional numbness. When depersonalization occurs in the context of trauma, individuals may turn to substances as a way to cope with the emotional void created by this dissociation. Let’s break down how depersonalization can lead to numbing through substance use:
1. Depersonalization as a Coping Mechanism:
- Emotional Overwhelm: Trauma often involves intense and overwhelming emotions that may be difficult to process. Depersonalization can serve as a defence mechanism, allowing individuals to disconnect from their emotions temporarily.
- Coping with Distress: Depersonalization can be a way for individuals to cope with the distressing thoughts and memories associated with trauma. By detaching from their own emotional experience, they create a buffer against the pain.
2. Creation of Emotional Void:
Numbing of Emotions: While depersonalization initially provides relief from intense emotions, it can result in emotional numbness over time. The detachment from emotions creates an emotional void, leaving individuals feeling numb and detached from their own experiences.
3. Substance Use as a Solution:
Seeking Emotional Relief: Faced with this emotional void, individuals may turn to substances such as drugs or alcohol to fill the emptiness and numb the emotional pain. Substances provide a temporary escape from the overwhelming feelings associated with trauma and depersonalization.
4. Cycle of Escapism:
Self-Medication: Substance use becomes a form of self-medication, offering a quick and accessible means of escaping numbness and emotional distress. This can create a cyclical pattern where individuals repeatedly turn to substances to maintain the numbness and avoid confronting the underlying trauma.
VEDA Rehabilitation and Wellness’ Holistic Approach:
VEDA Rehabilitation and Wellness stands as a beacon in the field of addiction treatment, particularly for the young population. Their holistic approach recognizes the multifaceted nature of trauma and addiction, offering a comprehensive set of strategies to address the unique needs of each individual.
1. Specialized Assessment:
VEDA begins by conducting specialized assessments to understand the unique experiences and traumas of each young individual. This personalized approach ensures that treatment plans are tailored to address the specific challenges faced by each person.
2. Integrated Therapeutic Modalities:
VEDA Rehabilitation integrates evidence-based therapeutic modalities, including individual and group therapy, trauma-focused cognitive-behavioural therapy, and creative arts therapies. These modalities help young individuals process trauma, build resilience, and develop healthier coping mechanisms.
3. Life Skills and Coping Strategies:
Understanding the vulnerability of the young population, VEDA places a strong emphasis on equipping individuals with life skills and coping strategies. This empowers them to navigate life’s challenges without resorting to addictive substances or behaviours.
4. Family Involvement and Education:
Recognizing the crucial role of familial support, VEDA involves families in the recovery process. Family therapy and education help create a supportive environment, fostering healing and strengthening relationships.
The correlation between trauma and addiction in the young population necessitates a nuanced and comprehensive approach to treatment. VEDA Rehabilitation and Wellness, with its holistic methodology, strives to address the intricate interplay between trauma and addiction in young individuals. By incorporating personalized assessments, evidence-based modalities, life skills training, and family involvement, VEDA empowers the population to embark on a journey of recovery that goes beyond the surface, nurturing holistic well-being and resilience for a brighter future.

