- Mumbai, New Delhi, Bangalore
- (+91) 81518 30000
- WhatsApp Now
- contact@vedawellnessworld.com
Addiction is a multifaceted condition that involves complex interactions between genetic, environmental, and neurological factors. Understanding the underlying mechanisms of addiction is crucial for developing effective treatments and interventions. One key concept that has gained significant attention in recent years is neuroplasticity. The role of neuroplasticity in understanding addiction, highlighting how the brain’s ability to change and adapt plays a central role in the development and persistence of addictive behaviors.
Neuroplasticity refers to the brain’s capacity to reorganize itself by forming new neural connections throughout life. This dynamic process allows the brain to adapt to new experiences, learn new information, and recover from injuries. Neuroplasticity can be both structural, involving changes in the physical structure of the brain, and functional, involving changes in how neurons communicate with each other.
Addiction primarily affects the brain’s reward system, which involves several key regions:
Central to the reward circuitry, the nucleus accumbens responds to pleasurable stimuli by releasing dopamine, a neurotransmitter associated with pleasure and reinforcement.
“A growing body of evidence suggests that nucleus accumbens (NAc) plays a significant role not only in the physiological processes associated with reward and satisfaction but also in many diseases of the central nervous system. Summary of the current state of knowledge on the morphological and functional basis of such a diverse function of this structure may be a good starting point for further basic and clinical research. The NAc is a part of the brain reward system (BRS) characterized by multilevel organization, extensive connections, and several neurotransmitter systems. The unique role of NAc in the BRS is a result of: (1) hierarchical connections with the other brain areas, (2) a well-developed morphological and functional plasticity regulating short- and long-term synaptic potentiation and signaling pathways, (3) cooperation among several neurotransmitter systems, and (4) a supportive role of neuroglia involved in both physiological and pathological processes. Understanding the complex function of NAc is possible by combining the results of morphological studies with molecular, genetic, and behavioral data”[2]
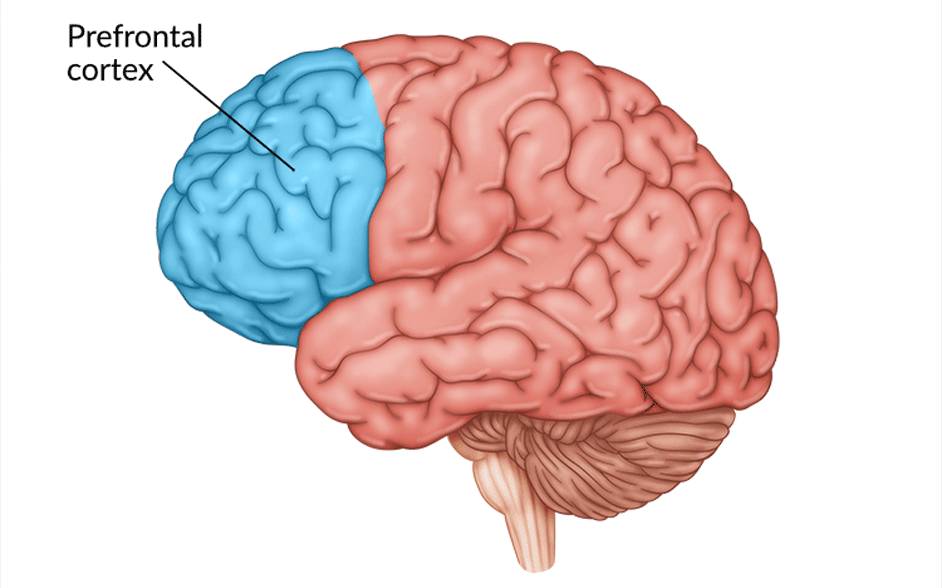
Responsible for decision-making, impulse control, and self-regulation, the prefrontal cortex helps individuals weigh the consequences of their actions and exert control over impulsive behaviors.
Involved in emotional processing, the amygdala plays a role in the formation of emotional memories and the response to stress and anxiety.
Neuroplasticity is a double-edged sword in the context of addiction. While it enables the brain to adapt and learn, it also contributes to the development and reinforcement of addictive behaviors. Here are some ways in which neuroplasticity influences addiction:
Repeated exposure to addictive substances leads to the strengthening of neural pathways associated with drug-related cues and behaviors. This reinforcement makes it more challenging for individuals to resist the urge to use substances.
Neuroplastic changes in the brain’s reward system contribute to tolerance, where individuals require increasing amounts of the substance to achieve the same pleasurable effect. This adaptation also leads to dependence, where the absence of the substance results in withdrawal symptoms.
Chronic substance use can impair the functioning of the prefrontal cortex, reducing an individual’s ability to make rational decisions and exert self-control. This impairment perpetuates the cycle of addiction, making it difficult to quit despite knowing the negative consequences.
Changes in the amygdala and other brain regions involved in emotional processing can result in heightened sensitivity to stress and negative emotions. Individuals may turn to substances as a coping mechanism, reinforcing the addiction.
Even after prolonged periods of abstinence, individuals can remain vulnerable to relapse due to long-lasting neuroplastic changes. The brain’s reward circuitry retains memories of drug use, making it easier for cravings and triggers to reignite addictive behaviors. This persistence underscores the importance of addressing neuroplasticity in addiction treatment.

Understanding the role of neuroplasticity in addiction opens up new avenues for treatment and recovery. Here are some approaches that leverage neuroplasticity:
CBT helps individuals identify and change negative thought patterns and behaviors. By promoting new ways of thinking and coping, CBT fosters the development of healthier neural connections.
Mindfulness practices, such as meditation and yoga, can enhance self-awareness and emotional regulation. These practices promote neuroplastic changes in brain regions associated with stress reduction and emotional control.
Regular physical exercise has been shown to promote neurogenesis (the formation of new neurons) and improve brain plasticity. Exercise also reduces stress and enhances mood, supporting recovery efforts.
Certain medications can help normalize brain function and reduce cravings. For example, medications like methadone and buprenorphine can stabilize brain chemistry and reduce the risk of relapse.
Engaging in new learning experiences and acquiring new skills can stimulate the brain and promote neuroplasticity. These activities can help individuals build a fulfilling life in recovery.
“SUD induces neuroplastic changes that predispose an individual to relapse and persist after completing SUD recommendations. Transcranial magnetic stimulation, environmental enrichment and exercise are shown to affect altered brain composition and reduce SUD-related negative behavior, while motor training appears to block neurophysiological changes normally caused by substance use. This illustrates that therapies targeting neuroplastic changes reduce adverse behaviors in those with SUD. The implementation of these modalities with current standard-of-care treatment may increase treatment success.”[1]